Population health exam 1 study guide
Exam 1 Assignment Guide (Learning Objectives, Additional Links)
Week 1: Population Health (16% of Exam, 8 Questions)
- Define health disparities, vulnerable populations & social determinants of health.
- health disparities: systematic, potentially avoidable health differences that adversely affect socially disadvantaged groups; distinct patterns of differences in health status and well-being across population groups; aka health inequalities
- vulnerable populations: individuals considered at greatest risk for poor health outcomes; e.g. poverty, racial/ethnic minorities, uninsured, children, elderly
- social determinants of health: the circumstances in which people are born, grow up, live, work, and age, as well as the systems put in place to deal with illness; often shaped by the distribution of money, power, and resources throughout local communities, nations, and the world
- Describe the goal of Healthy People 2020 & how it relates to health disparities.
- The goals of Healthy People 2020 are to (1) attain high-quality, longer lives free of preventable disease, disability, injury and premature death, (2) achieve health equity, eliminate disparities, and improve the health of all groups, (3) create social and physical environments that promote good health for all, and (4) promote quality of life, healthy development, and healthy behaviors across all life stages.
- Relationship to health disparities: research in a variety of areas has clearly indicated that health disparities are directly and indirectly linked to longevity and quality-of-life issues
- Identify the 5 components of social determinants of health. *mnemonic: SHEEN
- Social & Community Context
- Health & Health Care
- Economic Stability
- Education
- Neighborhood & Built Environment
- Identify and explain risk factors for vulnerable populations.
- risk factors for vulnerable populations: often politically marginalized in society; they experience discrimination and intolerance and may not have basic human needs met. The most consistent predictor of life expectancy, morbidity, mortality, and nearly all indicators of health status is low socioeconomic status
- Discuss health disparities and possible programs to help resolve them.
- Resolving Health Disparities through policy and programmatic interventions.
- federal policy: ACA, Medicare, Medicaid, Healthy People 2020
- state policy: Hoosier Healthwise; ISDH – Office of Minority Health which sponsors the “Minority Health Fair” & “Minority Health Conference”
- community programs: Marion County Health Department Vaccination Clinics, Paths to Quality
Week 2: Health Behaviors for Wellness (30% of Exam, 15 Questions)
- Describe different theories & their application to community/public health
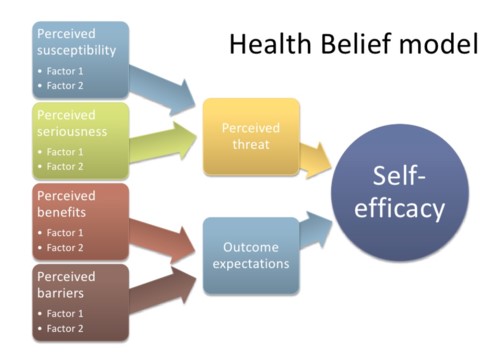
- Health Belief Model: analyze the probability to make changes to improve health; describes why some people take actions to prevent a disease and others don’t
- Individual perceptions
- Perceived susceptibility
- Perceived severity (of disease)
- Risk factors
- Perceived benefits of health action
- Perceived barriers
- Milio’s Framework for Prevention (complements HBM)
- Individual's ability to improve healthful behavior vs. society's ability to provide accessible options for healthy choices
- Proposed that health deficits often result from an imbalance between a population's health needs and its health sustaining resources; community-oriented, population-focused care
- Social Cognitive Theory (Social Learning Theory): to identify factors that affect certain health behaviors; a dynamic process in which personal factors, environmental factors & human behavior influence each other; self efficacy plays a big factor -- refers to an individual’s belief in being personally capable of performing the behavior required to influence one’s own health
- Observational learning – behavior acquisition that occurs by watching the actions and outcomes of others’ behaviors
- Reinforcements – responses to a person’s behavior that influence the likelihood of recurrence
- Reciprocal determinism – improvements in behavior influence self and others in continuing the behavior and vice versa with bad behavior
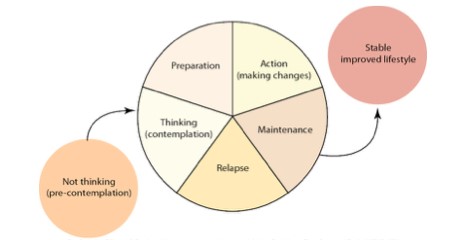
- Transtheoretical Model of Change (TMC): to plan health coaching or health teaching; useful for determining where a person is in relation to making a behavior change
- Precontemplation: No intention to take action in the next 6 months
- Contemplation: Intention to take action in the next 6 months
- Preparation: Have taken steps toward change; intends to take action within the next month
- Action: Has changed behavior within the past 6 months
- Maintenance: Has changed behavior for more than 6 months
- Termination: Self-Efficacy, behavior is permanent, relapse possible
- The Models in Relation to Health Coaching:
- Health Belief Model to me is what the internal conversation of the patient; severity, susceptibility, benefits, barriers, thinking of all this
- ...see where they are and guide them through
- Discuss the relationship of risk to health & health promotion activities
- Steps of Risk Assessment:
- hazard identification
- risk description
- exposure assessment
- risk estimation
- Health promotion tries to minimizes risk of a certain illness thru teaching
- Steps of Risk Assessment:
- Discuss the influence of health coaching on health & wellness
- health coaching: partnering with clients in a thought-provoking and creative process that inspires them to maximize their personal and professional potential
- health promotion: the art and science of helping people change their lifestyle to move toward a state of optimal health
- educating people about healthy lifestyles, risk education, self-care, developmental needs, activities of daily living & preventative
- health education: planned learning experiences based on sound theories that provide individuals, groups, and communities the opportunity to acquire the information and skills need to make health decisions
- involves providing info and facilitating health behavior changes
- List health behaviors for health promotion & disease prevention
- stress management: has been an effective intervention framework for health promotion, disease prevention & symptom management
- physical activity: decreases risk of death from heart disease, lowers risk for cancer, diabetes, HTN, depression, anxiety; promotes healthy weight, better sleep habits, improves mood and maintains cognitive function in the elderly
- sleep hygiene: essential in chronic disease prevention and health promotion
- Transtheoretical: Detailed Overview
- Transtheoretical and Diet Change
- Individual perceptions
- Health Belief Model: analyze the probability to make changes to improve health; describes why some people take actions to prevent a disease and others don’t
Week 3: Nutrition through the Lifespan (26% of Exam, 13 Questions)
- Summarize the basic nutrition recommendations in the Dietary Guidelines for Americans.
- Overarching Goals:
- Follow a healthy eating pattern across the lifespan.
- Focus on variety, nutrient density, and amount.
- Limit calories from added sugars, saturated fats and reduce sodium intake.
- Shift to healthier food and beverage choices.
- Support healthy eating patterns for all.
- Normal % of Daily Calories
- Carbohydrate (45% to 65% daily calories)
- Fats (20% to 35% of daily calories)
- Proteins (10-35% of daily calories)
- Calories per Gram
- Carbohydrates = 4 calories per gram
- Fats = 9 calories per gram
- Proteins = 4 calories per gram
- Identify the leading nutrition-related causes of illness and poor health in the US.
- CHD, CVA, HTN, cancer, osteoporosis, type ii diabetes mellitus, HIV/AIDS
- Explain and summarize nutrition recommendations for portion size, calorie, carbohydrate, fat, protein, vitamin and mineral intake.
- portion size: fruits and vegetables (size of woman's fist or baseball), meats (size of human palm or deck of cards), cheese (size of thumb or a six-die)
- calorie: provide calories or energy; carbs (45-65%) is 4 calories per gram, fats (20-35%) is 9 calories per gram, and proteins (10-35%) is 4 calories per gram
- carbohydrate: primary source of energy needed for CNS, kidneys, muscles, and brain to function properly; mainly found in starchy foods -- grains, potatoes, fruits, milk and yogurt; important for intestinal health and waste elimination
- fat: provides for normal growth and development, major source of energy, carries fat-soluble vitamins, cushioning for organs, makes things taste good, and slows down digestion (requires balance between fiber and fat)
- protein: complete → contains all amino acids needed such as milk, eggs, meats; incomplete → lacking 1+ amino acids such as grains, nuts, seeds; necessary for immune function, essential for tissue growth, repair, and maintenance
- vitamins: water soluble → B and C get filtered out quickly; fat-soluble → A, D, E, and K take longer to get filtered out (also why drugs last longer in system)
- vitamin D → sunshine
- vitamin B-12 → meat and dairy (animal products)
- minerals: major minerals → calcium, magnesium, potassium, sodium;
- Overarching Goals:
trace minerals → chromium, iodine, iron, selenium, and zinc
- iron supplements: pregnant women, HIV (certain diseases), elderly, anemic people, heart failure, GI disorders (malabsorption or GI surgery)
- iron should be taken immediately after meals
- zinc supplements: older adults, vegetarians, pregnant lactating moms, sickle cell disease, alcoholics
- potassium supplements: if loss due to illness or certain medications
- vitamins & minerals: required in small amounts; too many fat soluble vitamins can be dangerous and also too many minerals can lead to iron toxicity; play a unique role in maintaining health; the best way to get enough vitamins and minerals is to eat a balanced diet with a variety of foods; most people can usually get all the vitamins and minerals needed from the foods they eat
- Understand and apply food label contents to patient education.
- food label contents
- Use recommended sources of dietary information in teaching and coaching patients’ identified nutrition goals.
- Article on College Students Facing Hunger
- Article on School Lunch Programs
- 10 Rules for Reading Food Labels
Week 4: Coordination and Management (28% of Exam, 14 Questions)
- Define care coordination and related concepts.
- care coordination: set of activities organized by a team to facilitate appropriate delivery of necessary services; includes an inter-professional team including the patient, a proactive plan of care, target set of purposeful activities, practicing follow-up, and communication
- Describe the three models of care coordination.
- Social Model: addressed community and home-based needs (e.g. food and meal services for the elderly, utilities, assistance for low-income families, transportation assistance, etc.)
- Medically Oriented Model: addressed medical care (e.g. diagnosis- and provider-driven, case management to help navigate medical services, etc.)
- Integrated Model: combination of social and medical models, evolving to support a holistic, patient-centered and family-focused care
- Explain and use elements of communication.
- 3 Types of Communication:
- Linguistic: spoken or written words
- Paralinguistic: movement, appearance, expressions, gestures, eye contact
- Metacommunication: factors that compose the context of the message
- Effective Communication (LFSHiTS):
- Listening - focusing on message, reciprocity
- Flexibility - rules of appropriate communication
- Silence - can be therapeutic, lack of interest vs. reflection
- Humor - can relieve tension -or- can block communication
- Touch - can express concern, may be inappropriate or threatening
- Space - varies according to setting & culture
- Barriers of Communication (AAGRTS):
- Anxiety
- Attitudes
- Gaps (race, religion, age, language)
- Resistance
- Transference (reacting from previous experience
- Sensory gaps
- SBAR
- Situation
- Background
- Assessment
- Request/Recommendation
- advocacy: the act of speaking for others to assist them to meet needs; an expectation in the role of the professional nurse
- EHR: electronic health record, accurate and timely legal document
- 3 Types of Communication:
- Describe the context of a therapeutic relationship.
- therapeutic relationship: purposeful encounters characterized by effective communication; helping them to describe and clarify content and meaning, reflection, and constructive confrontation
- Characteristics of a Therapeutic Relationship:
- purposeful communication (goals)
- rapport
- trust
- empathy
- goal direction
- Describe how health literacy impacts self-management.
- health literacy: the capacity to read, comprehend, and follow through on health information
- Combat Health Illiteracy:
- use key clinical questions to teach people
- provide a safe, comfortable environment
- use therapeutic communication
- Effects of Health Illiteracy:
- prevents people from gaining full benefits of healthcare
- influences self-care abilities
- increases risk for poor health (health disparities factor)
- Explain how culture can impact self-management.
- Symptom vs Self-Management
- Symptom-management: ability of individuals and/or caregivers to engage in daily tasks required to maintain health and well-being
- Self-management: care provided for patients with life-threatening conditions; palliative care
- Culture’s Impact
- some may feel as if their culture holds higher importance than the management of their disease (e.g. Red Band Society when Jordy seeks medical treatment against the behest of his Mexican family)
- Article on Health Literacy
- Article on Self-Management
- Symptom vs Self-Management
-----
Helpful Assignment Tools
- https://quizlet.com/93014758/promoting-healthy-populations-exam-1-flash-cards/
- really thorough and includes pictures
- https://quizlet.com/153485905/b234-exam-1-material-flash-cards/
- another good detailed quizlet
- https://quizlet.com/186354491/b234-promoting-healthy-populations-exam-1-brandons-list-flash-cards/
- pretty straight forward answers, not sure if they’re right lol
-----
Practice Questions
- What is Healthy People 2020?
- Page 7 in Edelman describes Healthy People.
- The nurse in a newly opened community health clinic is developing a program for the individuals considered at greatest risk for poor health outcomes. The group is a:
- global community.
- local community.
- unmotivated population.
- vulnerable population.
- Rationale: Those who are vulnerable are individuals or groups that are at risk for exclusion from or lack of access to resources to maintain health.
- Which indicator is one of the most important determinants of the health of a nation?
- Infant Mortality Rates
- Rationale: Infant death is a measure of the health and well-being of children and the overall health of a community. It reflects the status of maternal health, the accessibility and quality of primary health care, and the availability of supportive services in the community.
- Life Expectancy Rates
- Mortality Rates
- Morbidity Rates
- Which statement accurately describe the Transtheoretical Model (TTM)?
- Sustained change over time occurs in the contemplation phase.
- Maintenance begins 6 months after the action has started, and may continue indefinitely.
- Rationale: Precontemplation: No intention to take action in the next 6 months; Contemplation: Intention to take action in the next 6 months; Preparation: Have taken steps toward change; intends to take action within the next month; Action: Has changed behavior/ modified lifestyle within the past 6 months; Maintenance: Has changed behavior & modified lifestyle for more than 6 months; Termination: Self-Efficacy
- When a person is considering the adoption of a change within the next 6 months, she or he is said to be in the precontemplation phase.
- In the contemplation stage, the individual has begun taking steps to make the change
- Health education is:
- those behaviors in which one engages with specific intent to prevent disease, detect disease in the early stages, or to max. health within the constraints of disease.
- This is Health Protection.
- Planned learning experiences based on sound theories that provide individuals, groups, and communities the opportunity to acquire the information and skills need to make health decisions.
- The art and science of helping people change their lifestyle to move toward a state of optimal health.
- This is Health Promotion.
- Stress can affect a person... (select all that apply)
- Physiologically
- Psychologically
- Spiritually
- Socially