Red flag rules for knee and lower leg differential diagnosis
EBP Presentation: Intubation
Scott Allen, Christy Brodzik, Nick Meyer
Class III: The soft palate and base of the uvula are visible. Class IV: The soft palate is not visible.
“LEMON” Assessment 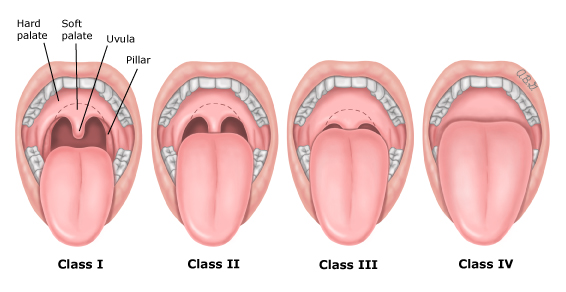
The LEMON Assessment has an 86% sensitivity and a 48% specificity when evaluating patients for difficult intubations (Hagiwara, Watase, Okamoto, Goto, & Hasegawa, 2015).
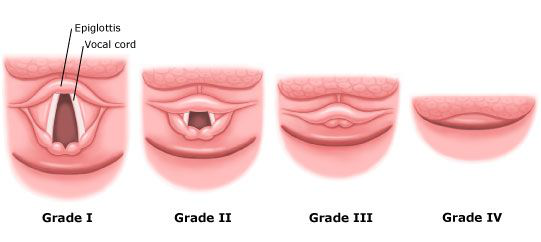
The Cormack and Lehane Score: There is a correlation between the Mallampati score. Grade I: Most of the glottis is visible.
•They examined common assessment tools like the Mallampati score, Thyromental distance, and upper- lip bite test.
•They reviewed 133 studies involving 844,206 adults and they found high variability in sensitivities, but high specificities among the most common bedside tests to detect airway management difficulty. •For detecting difficult airways, the upper lip bite test had the highest sensitivity (0.67, 0.45-0.83) and Mallampati test had the highest sensitivity of (0.51, 0.40-0.61) for detecting difficult intubation.
•Ultimately, clinical judgement, experiences, readiness, and vigilance are the best tools to be prepared when dealing with airway management. All of our patients will be different and each situation needs to be treated as such.
References
Roth, D., Pace, N. L., Lee, A., Hovhannisyan, K., Warenits, A. M., Arrich, J., & Herkner, H. (2019). Bedside tests for predicting difficult airways: an abridged Cochrane diagnostic test accuracy systematic review. Anaesthesia, 74(7), 915–928. doi: 10.1111/anae.14608
Evaluation of General Fitness for Scheduled/Elective Surgery Julie Bennett, Keith Harvey, Patrick Moran
Cardiac Review
1.Unstable Angina
2.Arrhythmias – chronic or new
3.Heart Failure – compensated/decompensated
4.Valvular disease – special concern for Aortic stenosis
5.EKG – indicated if +cardiac risk or > low-risk surgery
6.Echocardiogram – indicated for Hx of CHF & last Echo > 1 yr
7.Auscultation – heart sounds, vascular bruits, JVD, peripheral vasculature (may indicate occult coronary disease)Pulmonary Review
1.Airway – Mallampati Score (can be a good indicator of obstructive sleep apnea) 2.Asthma
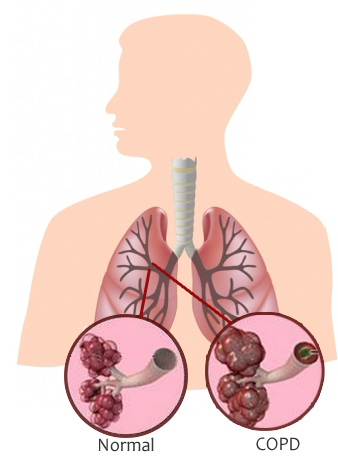
3.Smoking\COPD
4.Obesity
5.Obstructive sleep apnea
6.Pulmonary HTN
7.Upper respiratory infections
8.Metabolic & Nutritional factors (low albumin, <3.5 can predict perioperative pulmonary complications)
9.CXR - indicated if +cardiac/lung disease or >70 yrs old & no CXR in the past 6 months 10.Auscultation and visualization of respirations

EVIDENCED-
BASED
PRACTICE:
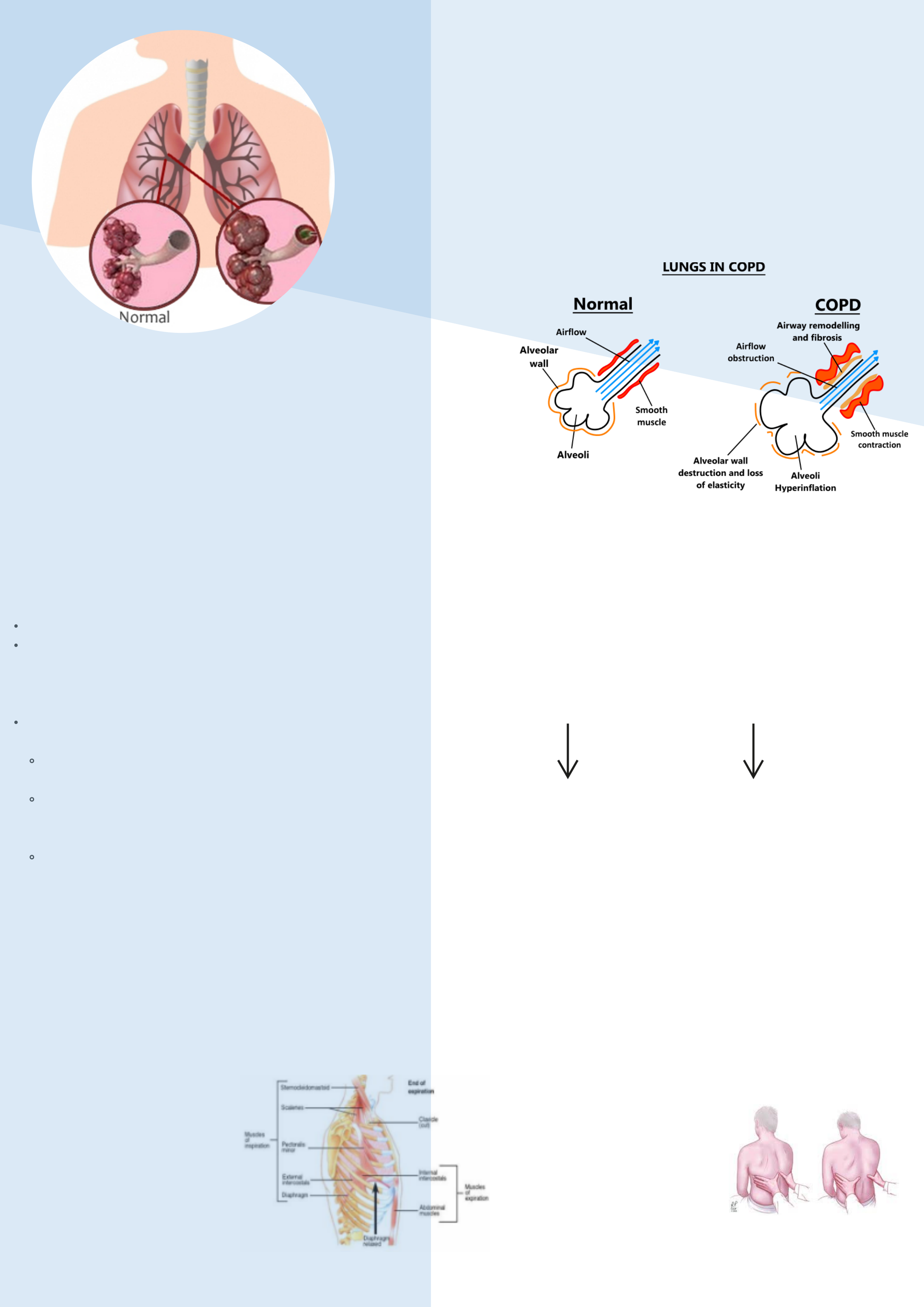
COPD- Childhood history
- Occupational History
- Familial/ Genetic History
- Red Flag: Smoking history
- Are you a current or former smoker? Have you been exposed to secondhand smoke?strategies to help with clinical recognition of physiological signs
Bedside elicitation of physical signs should always be the
starting point
| Physical diagnosis benefits: rapid, cost-effective, and can lead | ||
|---|---|---|
| to the earlier institution of various preventive and treatment | ||
| diagnostic modalities help to make earlier clinical diagnosis | ||
|
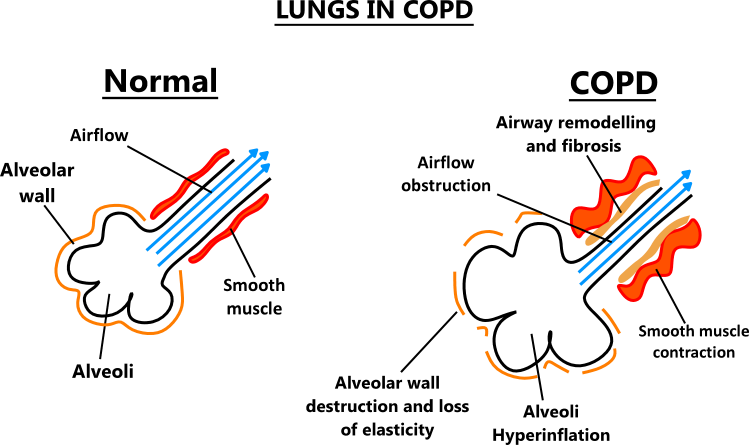
INITAL INSPECTION
- Low SpO2 (less than 92%)
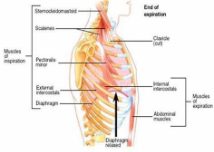
Acessory Muscle Phsyical Exam Components
- Do you have to stop and catch your breath during regular activities?- Do you have a cough?
- Do you have chest pain?
- Abnormal or “Positive Hoover’s Chest Sign” is an inspiratory indrawing of the lower lateral rib cage .
- Physical Exam: The Hoover's sign is examined by placing the first and second fingers on the costal margin near the
anterior axillary line.COPD patients may also show inspiratory indrawing of the lower sternum known as “anteroposterior ribcage paradox”
The sensitivity and specificity of Hoover's sign for the detection of airway obstruction is 58% and 86%, respectively, and the positive LR is 4.16 (Garcia-Pachon, 2002).
greater than its lateral diameter (1:1 Ratio)
|
||
|---|---|---|
|
||
|
||
|
||
|
||
| - PLB also increases recruitment of | ||
|
||
|
||
|
-Widened intercostal spaces
PERCUSSION
The percussion sound is a symmetrical,
a sensitivity of 20.8%, a specificity of
97.8%, and an LR of 9.5 (Oshaug et al.,
Asthma can be difficult for providers due to
similar historical and physiological exam
Lung cancer→ 8-10% prevalence of COPD is
reported with lung CA, both associated with
Chronic sinusitis→ inflamed or infected sinuses
can exacerbate COPD, leading to an increase
•Garcia-Pachon E. (2002). Paradoxical movement of the lateral rib margin (Hoover sign) for detecting obstructive airway disease. Chest, 122(2):651–655. doi: 10.1378/chest.122.2.651.
•Lamprecht, B., Soriano, J.B., Studnicka, M., Kaiser, B., Vanfleteren, L.E,. Gnatiuc, L.,…& Buist, S. (2015). Determinants of underdiagnosis of COPD in national and international surveys. Chest, 148(4), 971– 985. doi: 10.1378/chest.14-2535
•Mattos, W.L., Signori, L.G. , Borges, F.K., Bergamin, J.A., & Machado, V. (2009). Accuracy of clinical examination findings in the diagnosis of COPD. J Bras Pneumol, 35(5), 404-408. doi: 10.1590/s1806-
37132009000500003
•Mayo Clinic (2020, April 15). COPD.
Pneumonia: inflammatory response of the bronchioles and alveoli to an infective agent
History and Physical Exam Elements
Combined multiple predictors for improved diagnostic accuracy: fever
>37.8°C, heart rate >100 beats per minute, decreased breath
sounds, crackles:
•If prevalence is 5%:
oAll predictors present → probability of pneumonia is 53%
oIf these 4 predictors are absent → probability of pneumonia is 1%
Factors Affecting Exam Technique and Interpretation
(Douglas et al., 2014)
•Human Error – language barrier, fatigue, stress
•Experience – lack of skills/knowledge
•Location – remote clinical area versus busy clinical area (no
help/interruptions) •Equipment – reliance on technology
•Time/Pressure – patient decompensating
Kelsberg, G., & Safranek, S. (2003). How accurate is the clinical diagnosis of pneumonia? The Journal of Family Practice, 52(1) Retrieved from
https://www.mdedge.com/familymedicine/article/60101/infectious-diseases/how-accurate-clinical-diagnosis-pneumoniaMoberg, A. B., Taleus, U., Garvin, P., Frannson, S. G., & Falk, M. (2016). Community-acquired pneumonia in primary care: clinical assessment and the usability of chest radiography. Scandinavian Journal of Primary Health Care, 34(1), 21-27.
Adam Conrad, Lashlee Lacerna, Jessi Ponder, James Reichert
Introduction: Irregular clotting factors or time and quantity can lead to venous thromboembolism. Clots in veins generally occur in
1–3). Patients with DVT may have varied clinical presentation and may even be asymptomatic (Kim, 2019).
Red Flags
● Decreased blood flow often caused by inactivity or immobility (ASH, 2018).
● Increased estrogen: birth control pills, pregnancy, hormone replacement therapy (ASH, 2018).
2017).
● Another study found Homan’s sign was more common in patients with a negative venogram than a positive one (Ambesh et al.,
● Venography - GOLD STANDARD (Centers for Disease Control and Prevention [CDC], 2020).
○ Contrast is injected into a large vein in the foot/ankle under X-ray so the deep veins in the leg up to the hip can be
○ Best Non-Invasive Diagnostic Method; Standard imaging used to detect DVT. Has all but replaced contrast
venography (CDC, 2020).
■ Part 2: Uses sound waves to detect changes or absence of blood flow
● D-Dimer
https://doi.org/101016/j.ihj.2017.01.013
American Society of Hematology. (2018). Understanding blood clots [Infographic]. ASH Clinical Practice Guidelines On Venous
Centers for Disease Control and Prevention. (2020). Diagnosis and treatment of venous thromboembolism.
https://www.cdc.gov/ncbddd/dvt/diagnosis-treatment.html
Kim, Y. J. (2019). Red flag rules for knee and lower leg differential diagnosis. Annals of Translational Medicine, 7(7). doi:10.21037/atm.2019.07.62
Kushner, A., West, W. P., & Pillarisetty, L.S. (2019). Virchow triad. STATPEARLS. https://www.ncbi.nlm.nih.gov/books/NBK539697/
https://doi.org/10.1136/bmj.326.7400.1180
Zitek, J.A., Baydoun, J., & Baird, J. (2013). Tools for the clinician: Essentials of bedside (ED or ICU) ultrasound for deep vein thrombosis. Current





