Example the kolbs and gibbs reflective cycle gibbs
Introduction
This essay has asked me to reflect on the importance of professional values & care in healthcare, to achieve this this essay will review a carefully selected real life case study experience of a dementia patient within a hospital setting, the aim is to extrapolate from this case study the impact of professional conduct on patient’s health care pathway experience.
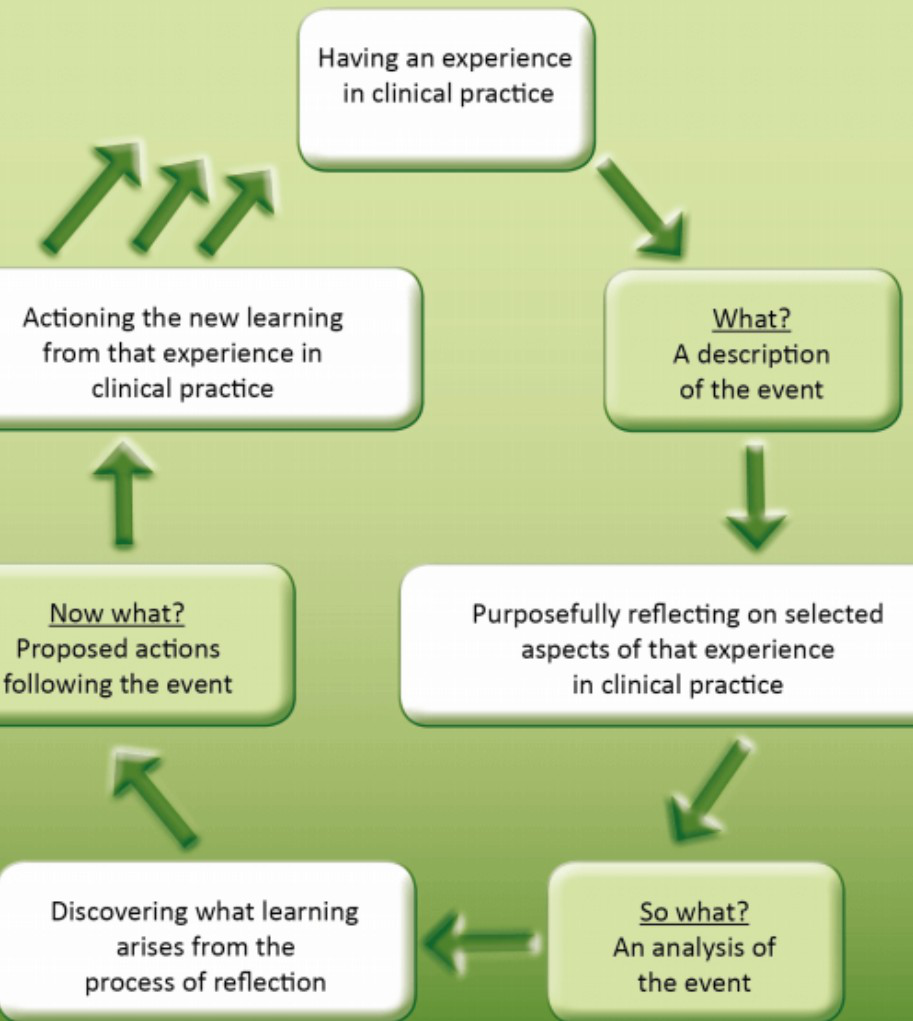
However, to achieve the target of this essay which is to reflect on the“What” the “So What” and the “Then What”, This essay will be utilising the most effective model tailored to achieve the above-mentioned areas of reflection. This essay will focus on an the Hugh;s hospital situation using the critical reflection of series of incidents encountered in practice. This will be achieved using Drisdol’s (2007) model of reflection.
Reflective practice in healthcare in general and nursing in particular is important as it promotes improvements in their clinical and managerial practice. Reflective practice is one of the most effective ways to transform theory into practice in the healthcare setting (Koshy et al, 2017). To this end, for one to reflect effectively, there is need to use one of the many models for reflections but the general gist of most reflections is to focus on “what happened, why does this matter, and what are the next steps?”(Koshy et al., 2017).
Reflection is, therefore, a mechanism of analysing an experience with a view to learn from practice, that is, learning by doing (Gibbs, 1988) and it is in line with the requirements of the NMC (2018) for all nurses to utilise feedback to introspect on how to improve on the performance of their duties. In this regard, there are several models for reflection that include Kolb’s (1984) Model of Experiential learning that centres on the concept of nurturing understanding through actual experiences; Gibbs’ (1988) Reflective Cycle; Driscoll’s (2007) What Model; and Jasper’s (2013) Experience, Reflection and Action (ERA) model. This reflection uses Driscoll’s (2007) model, which is premised on three questions namely What, So what and Now what? (Driscoll 2007). These questions enable practitioners to scrutinise their experiences and to learn from them (University of Cambridge, 2020).
Hugh is a mental patient with diminished faculties as a result of dementia and his health continued to plummet while in hospital, resulting in severe confusion and aggressive behaviour. The fact that no one at the healthcare facility knew what was really happening to Hugh shows that there was a lack of proper diagnosis of the real disease afflicting Hugh due to lack of a multi-disciplinary team input. According to the World Health Organisation (WHO) (2019), dementia is associated with diminished memory, thinking and behaviour. However, Hugh was also a victim of the war and this might have had some psychological impacts on him (REF).
According to WHO, approximately 10 percent of people who undergo traumatic events will develop serious mental health challenges while another 10 percent will develop behaviour that terribly affects their ability to function properly (WHO, 2001). As a result, the victims, such as Hugh who was evacuated during the war, suffer from conditions such as anxiety, depression and other psychosomatic challenges like insomnia (WHO, 2001). What this means is that Hugh should have undergone thorough mental and psychiatric examination to rule out possibility of schizophrenia or post-traumatic stress disorder (PTSD), which – according to Mayo Clinic (2020) is a “mental health condition that’s triggered by a terrifying event – either experiencing it or witnessing it [and] symptoms may include flashbacks, nightmares and severe anxiety, as well as uncontrollable thoughts about the event”. Hugh is exhibiting some of these symptoms but the healthcare providers did not know exactly what was happening to him because not thorough investigation had been done
The nursing staff did not properly communicate with Barbara to discuss Hugh’s health and ways to manage the same, resulting in Barbara getting stressed in connection with the hospital discharge process, which was purported to include an assessment of Hugh’s mental capacity and ability to provide consent or power of attorney. No proper detection had been done for Hugh so no effective treatment was being administered hence the basis of effective and therapeutic communication did not exist and this explains why Barbara was failing to cope.
2.2 So What?
The concept of whistle-blowing in nursing practice promotes openness, accountability and transparency by enabling healthcare institutions to learn from past events as a way of preventing the recurrence of similar incidents or concerns, which ultimately results in improved patient safety and care (NMC, 2015). It, therefore, follows that had a nurse blown the whistle on the ill-treatment of Hugh and his wife, some of the harm that occurred to the patient would have been prevented. Ethical conduct requires nurses to play the role of patient advocacy to ensure patient safety by whistle-blowing, although research suggests that this is risky as nurses risk demotions, threats, peer rejection, pressure to resign and being labelled a sell-out (McDonald & Ahern, 2000).
The research by McDonald and Ahern (2000) showed that there were serious professional repercussions if the nurse came forward to blow the whistle wrongdoing while quiescence was associated with few professional implications. To encourage nurses to protect patients against the incompetence of fellow healthcare professionals as part of advocacy, some nursing associations have come up with guidelines, such as the Finnish Ethical Guidelines for Nurses (1996) cited in McDonald and Ahern (2000) that stipulates that every nurse shall be responsible for guaranteeing that no healthcare professional acts unethically when dealing with patients.
A multidisciplinary team was very essential to handle Hugh and it should have comprised of nurses, psychiatrist, physician, nurse aides (to ensure the patient’s cleanliness and hygiene), the wifeand a social worker, among other important team members. It is well-documented that a multidisciplinary approach promotes better healthcare outcomes (Hughes, 2018). In this regard, doctors, nurses and other health professionals work together and share resources and information for the betterment of the patient’s health (Hughes, 2018). As such, a multidisciplinary team would have made a comprehensive assessment of Hugh’s situation and then implemented a full-gamut treatment plan (Hughes, 2018).
The ethical principle of beneficence was violated in the Hugh case as it states that healthcare providers must do all they can to benefit the patient in each scenario yet nothing was done. In addition, the ethical principle of non-maleficence was not followed as it means to do no harm” (Saint Joseph University, 2020) as some of the decisions
It is recommended that grants should be availed to academics for continuous research on professionalism in nursing with special focus on communication, whistle blowing, mental health patients’ care, family involvement in healthcare delivery as well as values, principles and ethics in healthcare delivery.
is a 78 years old man diagnosed with dementia, it will explore the Recently his condition has deteriorated, and he has presented at the hospital with
made Barbara upset, as Hugh is known to be meticulous about his personal hygiene. Hugh has now been placed on puree diet following the recent disappearing of his dentures, which has made eating solid food a struggle a for him, consequently he has started to refuse food very often.
Barbara has requested to stay with him, but the staff said she couldn't because it would be disruptive for the other patients and there would be nowhere for her to sit. Two days later, Barbara got a phone call to say that Hugh had slipped over the cot sides and was badly bruised. This was deeply upsetting for her. Discussions surrounding Hugh’s discharge involved assessing his mental capacity and ability to provide power of attorney, was a very stressful one to Barbara as she hasn’t done this before.
for continuous learning on professional conduct and its application in the work environment), attitudinal (the attitudes and notions that give guidance to nurses in the execution of their duties, such as the propensity to be flexible to achieve what is good for the patient), as well as psychomotor (sharpening of skills through practice in order to improve self-discipline).
Professionalism in nursing, therefore, refers to “a set of values that are critical to elevating the quality of patient care while improving the methods, standards, and judgments that guide nursing practices every day” O'Connor et al (2020), (Regis College, 2020 ??????). To this end, professionalism in the nursing field entails the provision of quality patient care by prioritising patients, efficient practice, the preservation of safety, and promotion of trust as stipulated in The Code for United Kingdom (UK) nursing practice (NMC, 2018). The Code plays an instrumental role in guiding nurses, midwifes and nursing associates for them to carry out their duties in a professional way that is premised on the adherence to values such as respect, advocacy, compassion, dignity, care and responsibility (Regis College, 2020; NHS Constitution, 2015). The importance of professionalism in healthcare in the United Kingdom was also expounded in the NHS Constitution (2015) as the National Health Services “aspires to the highest standards of excellence and professionalism”.





